What is Urodynamics
Urodynamics is a study to assess the function of urinary bladder , sphincters and urethra in two important phases of micturition i.e. Storage and Emptying and thereby helping as an adjunct tool in diagnosing the pathology.
Today, the urodynamic armamentarium is
- Uroflowmetry
- Cystometry
- Pressure-flow studies
- Electrophysiologic studies
- Urethral pressure studies, and
- Videourodynamic studies
Nitti noted three important principles in urodynamics
- A study that does not duplicate the patient's symptoms is not diagnostic
- Failure to record an abnormality does not rule out its existence, and
- Not all abnormalities detected are clinically significant ( Nitti and Combs, 1998 )
Aim of Urodynamics
The aim of clinical urodynamics is to reproduce symptoms while making precise measurements of the bladder physiology.
INDICATIONS and Selection of Patients for Conduction of Urodynamics
- Patients in whom potential therapy may be hazardous where one would want to be sure of the correct diagnosis before instituting therapy
- Patients with recurrent incontinence in whom surgery is planned
- Patients with incontinence and a confusing mix of stress and urge symptoms and those with associated voiding problems
- Patients with neurologic disorders and those with a mismatch between symptoms and clinical findings Patients with LUTS suggestive of bladder outlet obstruction
- Patients with LUTS who have both obstructive and marked instability symptoms
- Patients with obstructive LUTS and neurologic disease - Young men with LUTS
- Neurologically impaired patients who have neurogenic bladder dysfunction
Preparation of Patient
- Prestudy discussion of the study technique and counseling about the risks are appropriate
- History and physical examination
- During the study, the patient should understand what information we are trying to collect sufficiently to be able to volunteer timely responses to changing events.
- Urine c/s : no growth
- Bowel preparation
The Urodynamics Room
- The room used for urodynamics should be without distractions, quiet, and protected from unnecessary interruptions.
- The room should be large enough for the physician
- To perform a physical and pelvic examination,
- To place catheters, and
- To move unencumbered within the room
- One should always take into account the need for sufficient room to allow for wheelchairs and assist devices such as walkers.

Urodynamic Equipment
- Three measurement channels
- Two for pressure and
- One for flow;
- A display (on either a printer or a monitor); and
- A method for secure storage of the recorded pressures (abdominal, vesicle, detrusor) and
- Flow measurements as tracings against time ( schafer et al, 2002 )
Catheters
- The standard catheter for routine urodynamics is a transurethral, double-lumen catheter.
- This allows the fill and void sequence to be repeated without recatheterization.
- Similarly sized triple-lumen catheters are available that allow bladder filling, intravesical pressure measurement, and urethral pressure recording.
- The use of a balloon catheter is best for the measurement of abdominal pressure.
- An air-free balloon in the rectum or in the vagina in women
- The balloon maintains a small fluid volume at the catheter opening to avoid fecal blockage preventing pressure transmission
Types of Flowmeter
- Gravimetric flowmeters operate by measuring the weight of the collected fluid or by measuring the hydrostatic pressure at the base of the collecting cylinder.
- The electronic dip stick flowmeter measures the electrical capacitance of a dipstick mounted in a collecting chamber.
- In the rotating disk flowmeter the voided fluid is directed onto a rotating disk. The power required to keep the disk rotating at a constant rate is measured and proportional to the mass flow rate of the fluid.
- Today, most available flowmeters are gravimetric or rotating disk transducers.
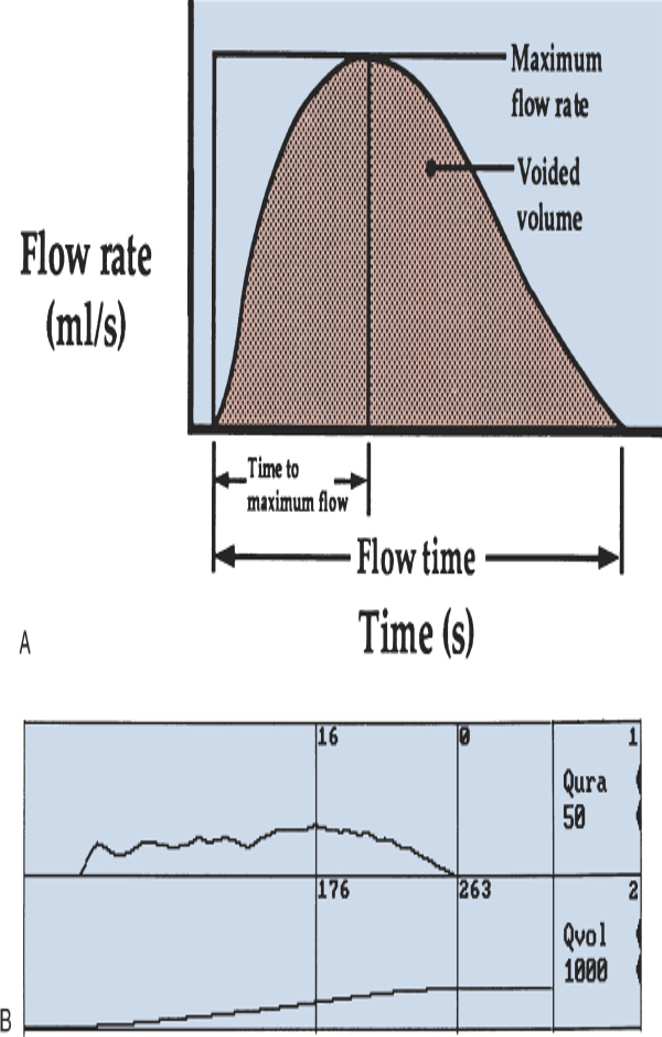
Uroflow
- Uroflowmetry is noninvasive, inexpensive, and invaluable in screening patients with voiding dysfunction.
- This noninvasive test should precede any other urodynamic studies.
- It is easy to perform and quickly provides data on both storage and voiding symptoms.
- Ideally, two or more tests should be performed, and the addition of a noninvasive postvoid residual volume measurement by ultrasound adds to the value of the study.
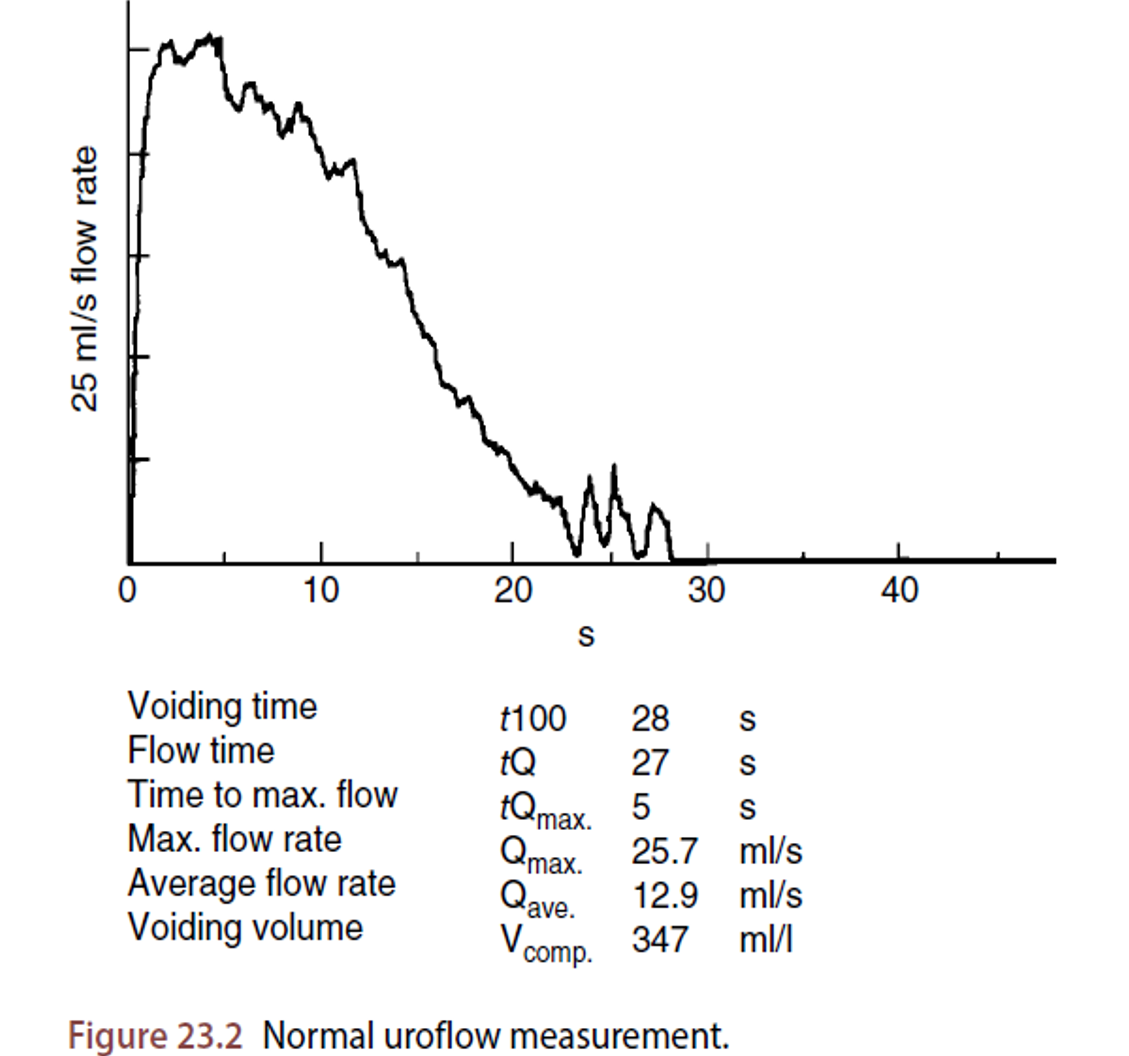
- The normal flow pattern is a continuous, bell-shaped, smooth curve with a rapidly increasing flow rate
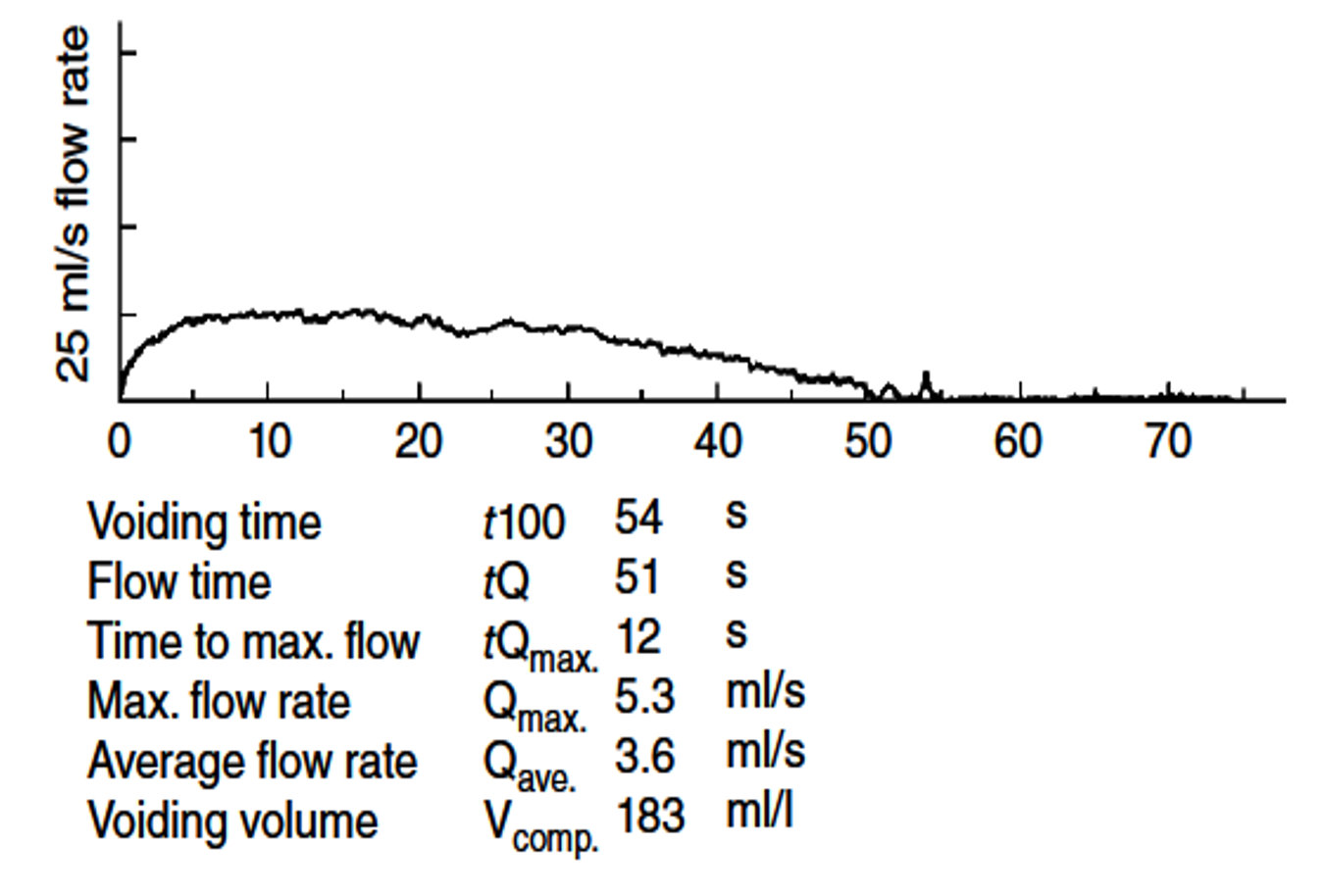
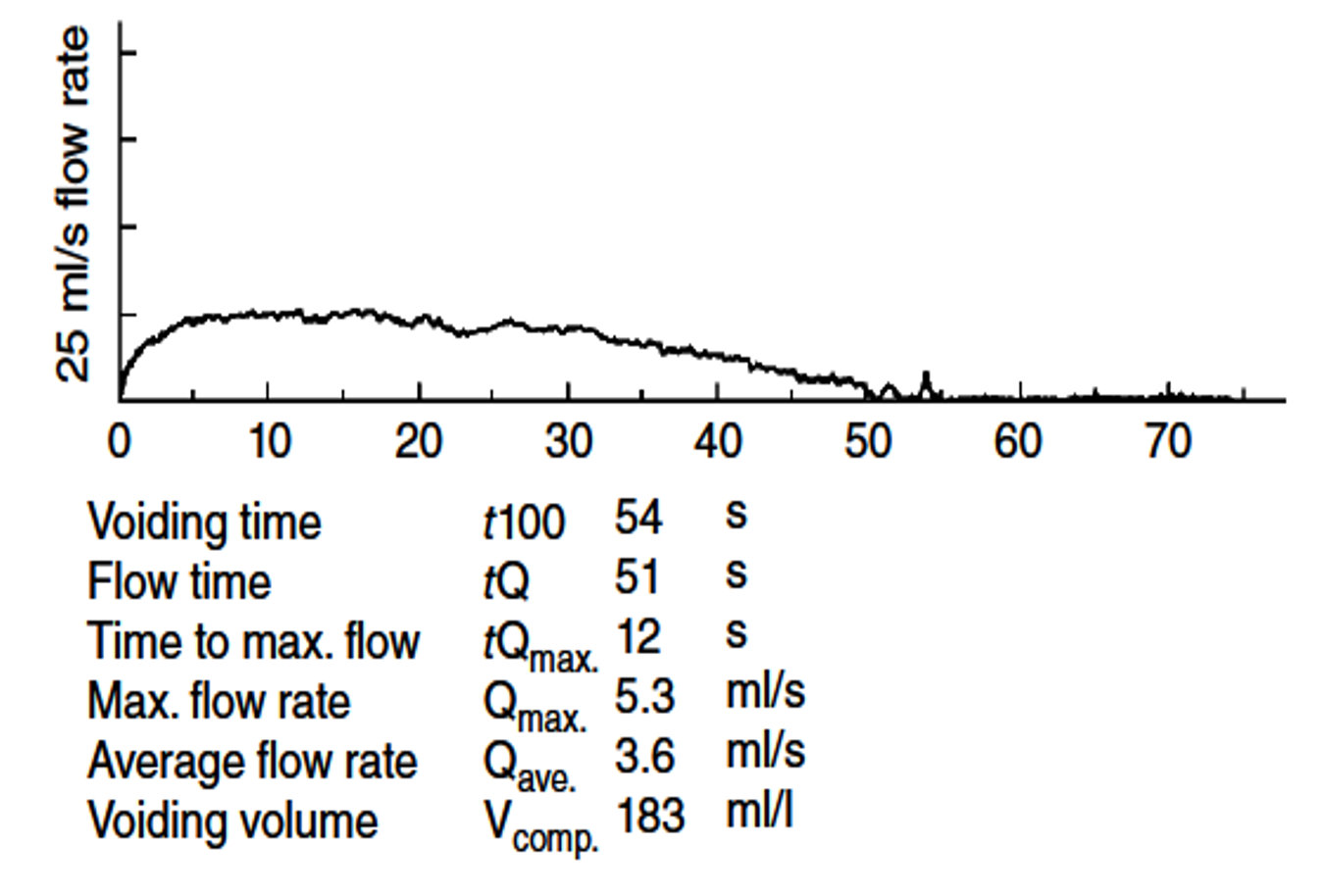
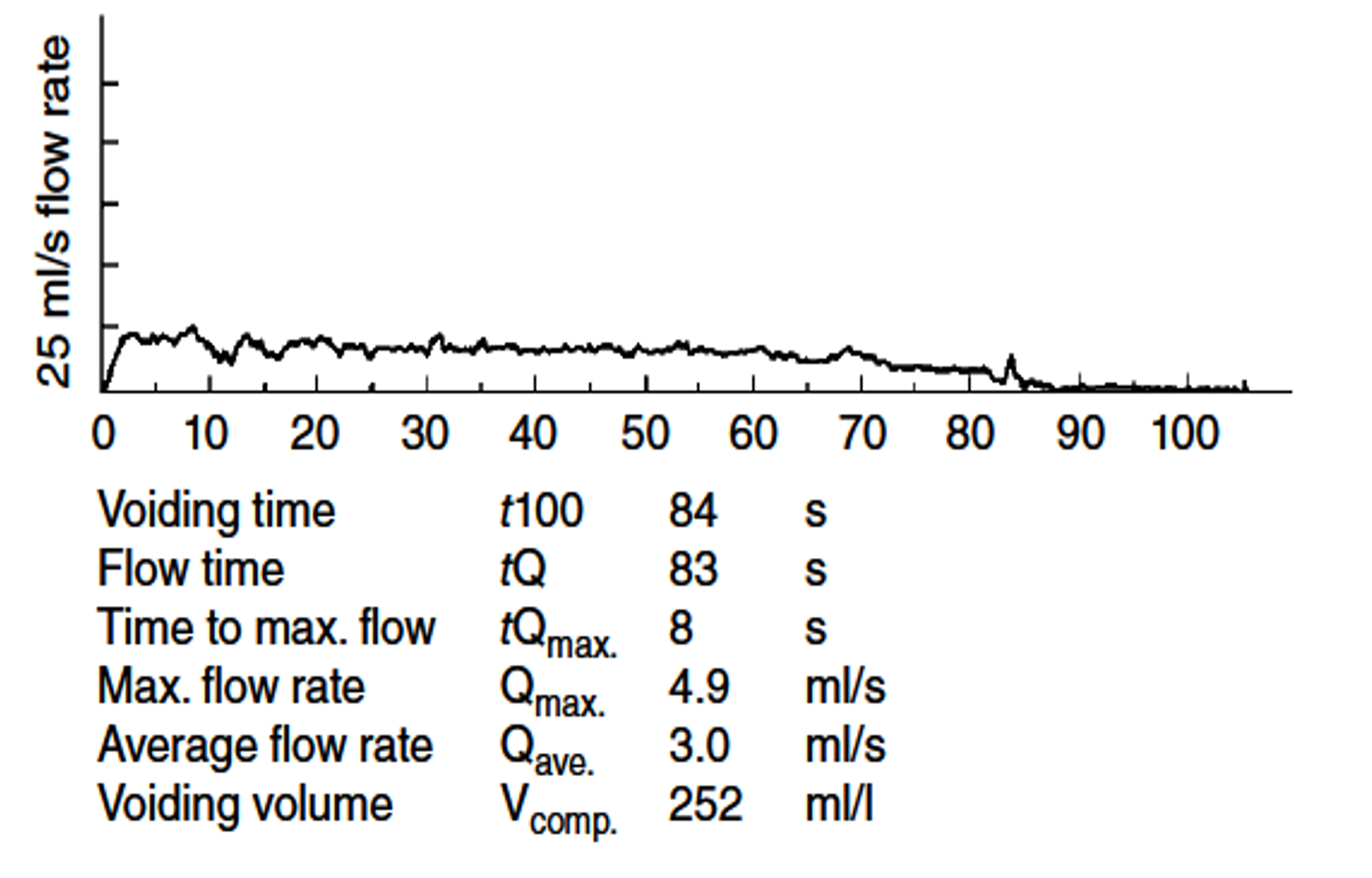
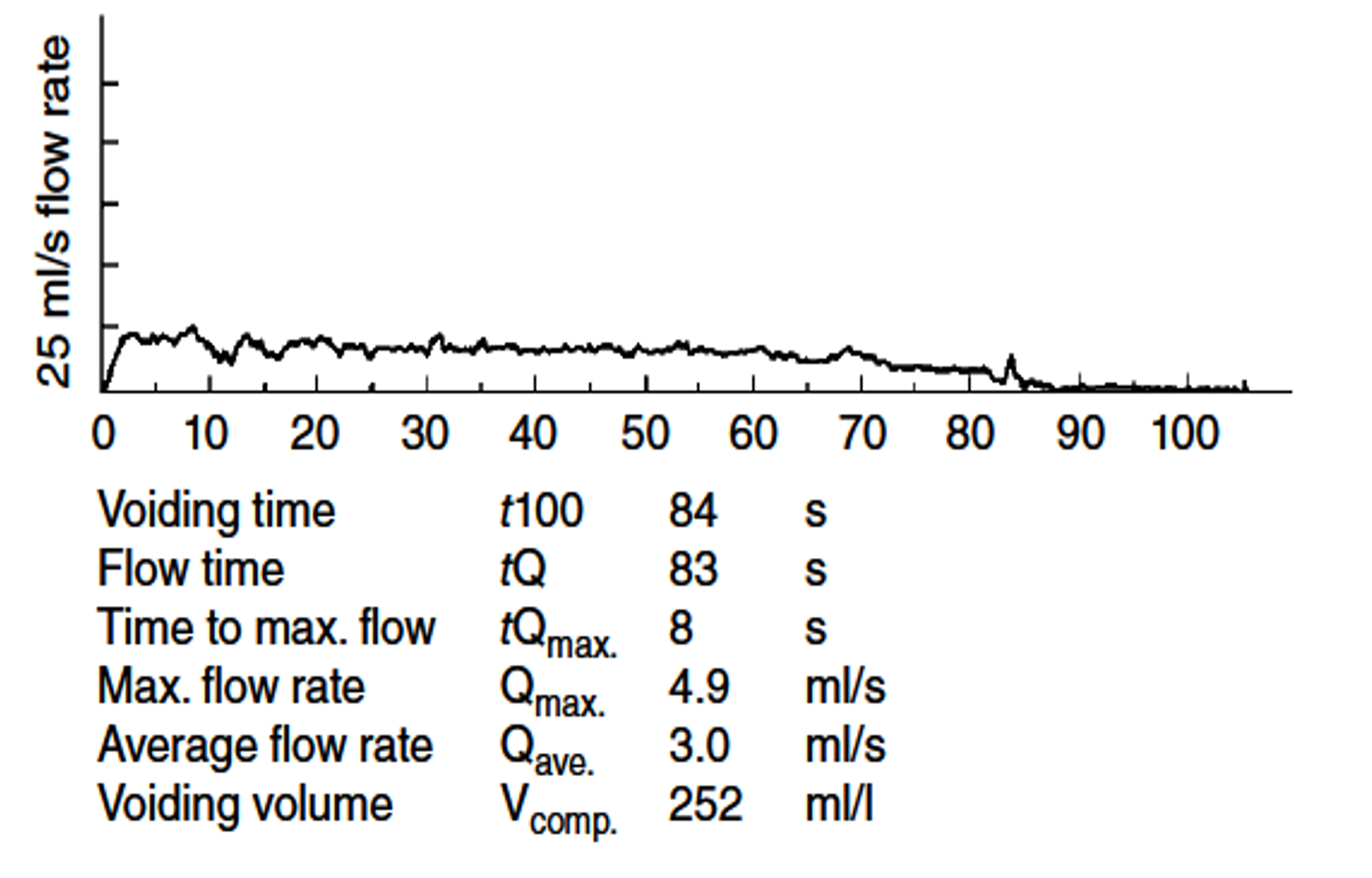
- The typical obstructed flow pattern has a plateau-shaped curve with a prolonged flow time, sustained low flow rate, and increased time to Qmax.
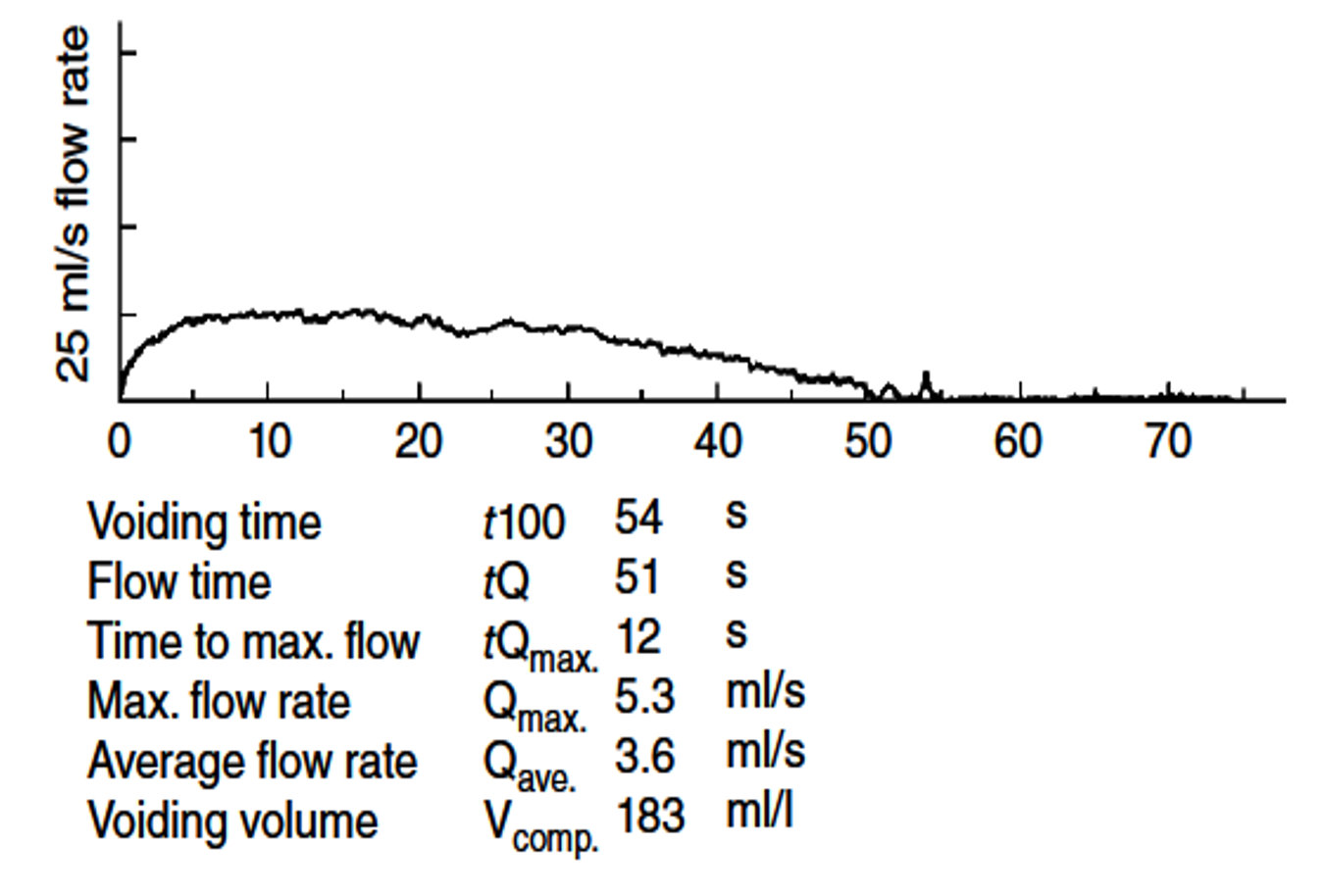
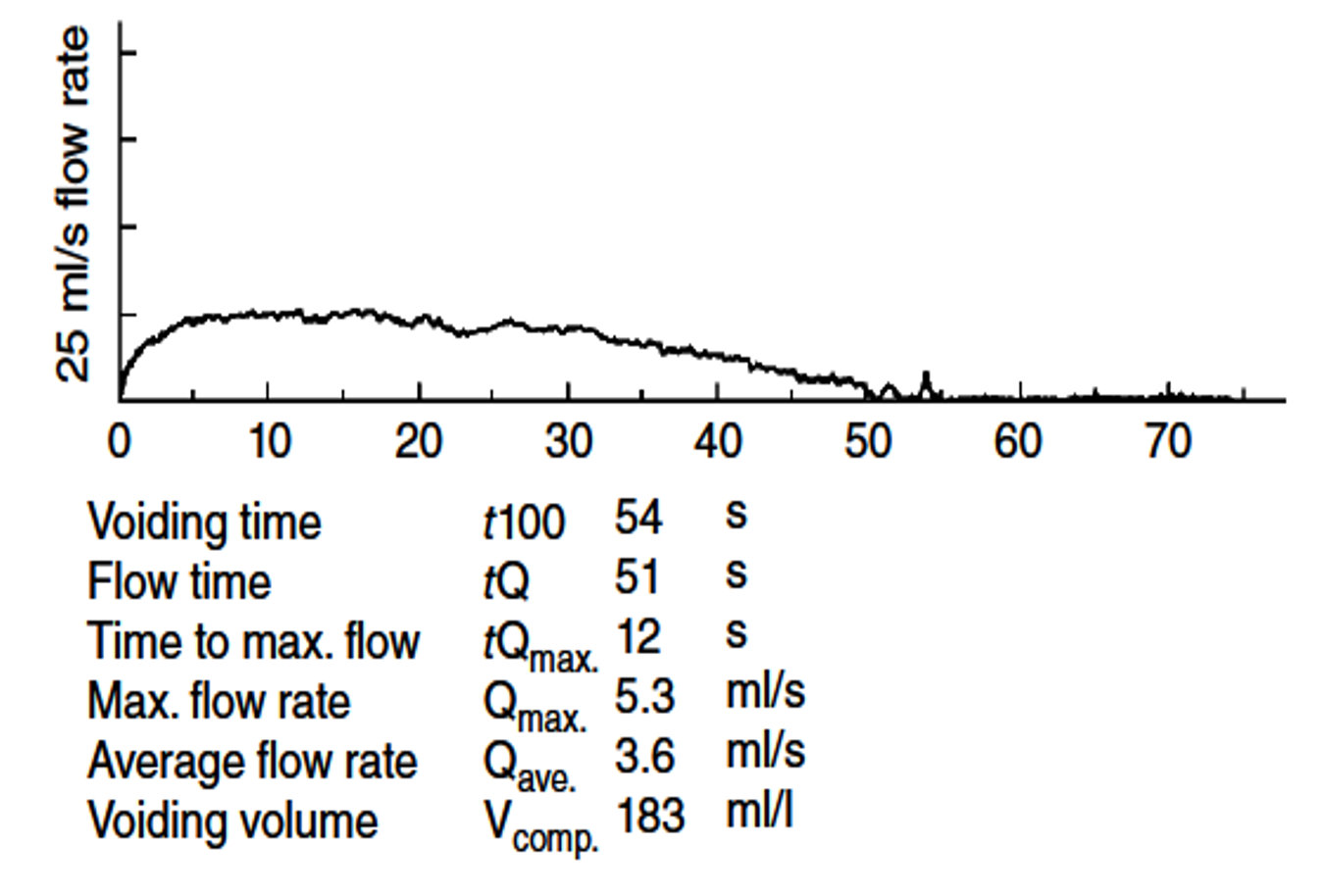
- An intermittent flow pattern is one that has one or several episodes of flow increasing or decreasing (or ceasing completely) and is commonly secondary to abdominal straining or external sphincter spasm (e.g., detrusor-sphincter dyssynergia).
Obstructive flow pattern due to prostatic enlargement
Obstructive and a FIXED flow pattern due to Urethral Stricture
Intermittent flow pattern e.g. Dysfunctional voiding
The Procedure
- Measurement of Intravesical and Abdominal Pressure.
- Zero pressure is the surrounding atmospheric pressure.
- The reference point is the superior edge of the pubic symphysis
- All systems must be zeroed to atmospheric pressure, and it is crucial that there are no air bubbles in any of the transducers or tubing as these may cause pressure dampening or dissipation.
- Prior to filling, we prefer to conduct a noninvasive uroflow test as described earlier.
- The patient is then catheterized for a postvoid residual at the time of cystometry catheter placement.
- During cystometry, periodic coughing should be elicited to ensure accurate pressure recording in all channels being monitored (Pdet as derived from Pves and Pabd).
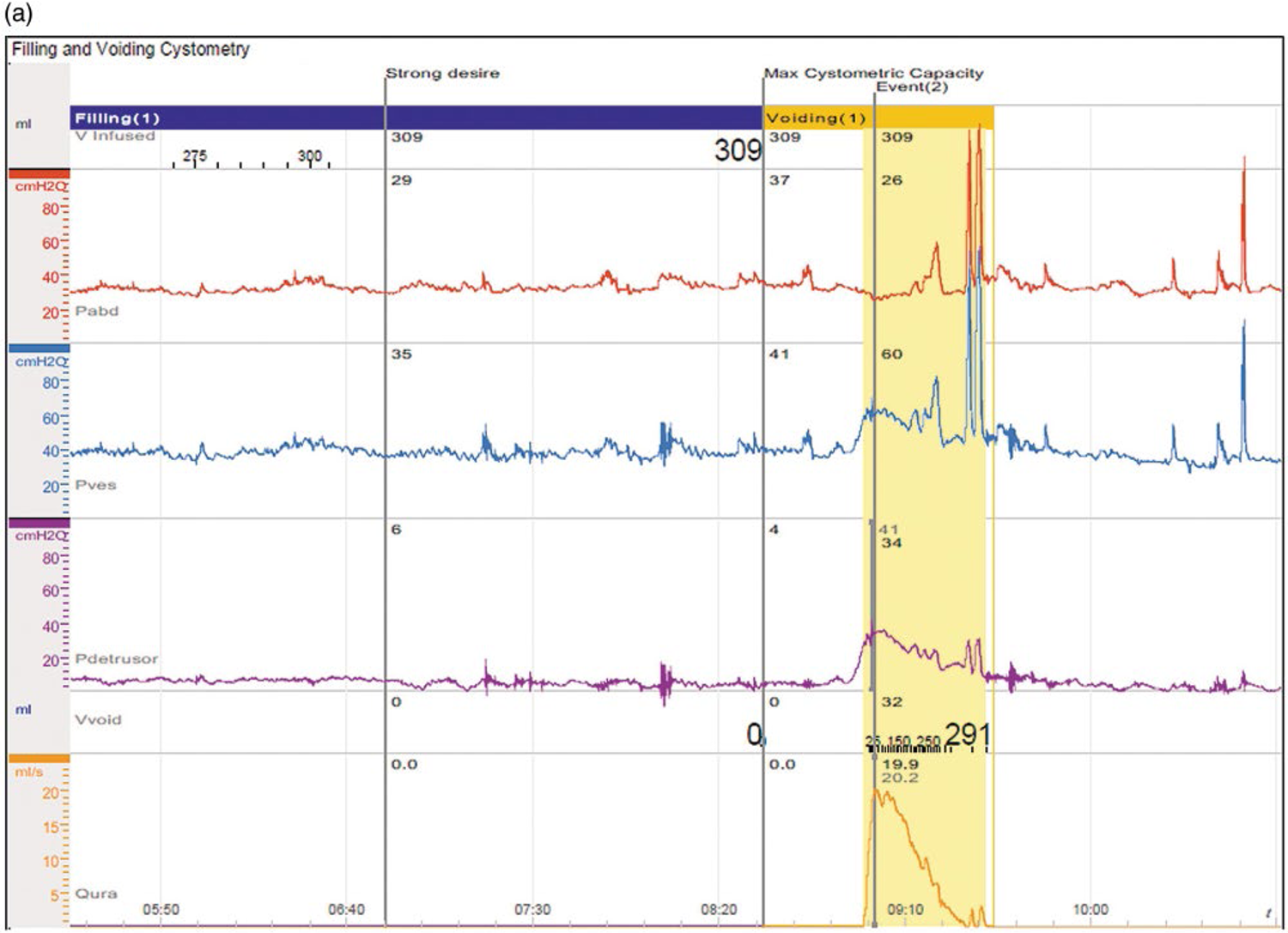
Filling Cystometry
- During the course of cystometry
-
Four bladder characteristics
- Capacity,
- Sensation,
- Compliance, and
- The occurrence of involuntary contractions.
Capacity
- Maximum cystometric capacity bladder volume at the end of the filling CMG when patients have a strong desire to void, feel they can no longer delay micturition, and are given permission to void . This volume includes 1.the amount voided and 2.the residual urine left after the void (postvoid residual).
- The functional bladder capacity is the largest volume voided as determined by a voiding diary.
- The cystometric capacity is usually slightly greater than functional bladder capacity
Sensation
- Bladder sensation is evaluated by questioning the patient about the feeling of the degree of bladder fullness and is the point at which cooperation between the patient and examiner becomes very important.
-
Normal bladder sensation
- The first sensation of bladder filling
- The first desire to void, and
- A strong desire to void
- Urgency,
- Pain, and
- Multiple other sensations should be documented during filling as well
Compliance
- Bladder compliance is the relationship between change in volume and change in pressure.
- It is generally calculated between two points:
- the Pdet with the bladder empty at the start of filling and
- the Pdet at either the maximal cystometric capacity or the start of a detrusor contraction.
- Normal bladder compliance should be less than 12.5 mL/cm H2O.
9 C’s of Urodynamics
-
FILLING phase
- Contractions (detrusor oceractivity)
- Compliance (normal / poor )
- Continence (Stress / Urge / Mix)
- Coarse Sensation (Normal / Reduced)
- Cystometric capacity
-
VOIDING phase
- Contractions (Pdet = contractile / hypo / hyper)
- Complete voiding (check for post – void residue)
- Coordination (Vesicourethral)
- Clinical obstruction
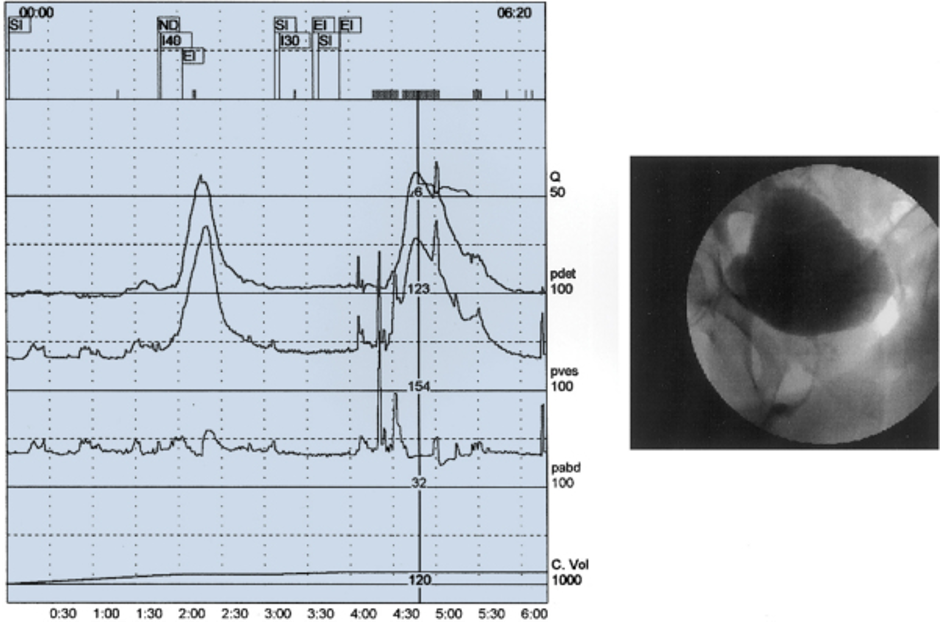
Videourodynamics
- Definition: The simultaneous display of bladder and urethral pressures with fluoroscopic imaging of the lower tract is videourodynamics.
- It is the most sophisticated form of evaluation of patients with complex urinary tract dysfunction.
- This is desirable when simultaneous evaluation of structure and function is necessary to make a diagnosis
- Videourodynamics is useful to identify the specific site of the obstruction as being at the bladder neck, the prostatic urethra, or the distal sphincter mechanism
