Introduction
Incontinence is the leakage of urine or stools. Bowel incontinence is sometimes called faecal incontinence or anal incontinence. It is the uncontrolled loss of solid or liquid stools, or wind (gas) with leakage.
Bowel incontinence is often a distressing problem. It varies in severity from mild difficulty controlling gas (wind), to loss of control over liquid and solid stools.
Bowel incontinence can affect anyone, but it is much more common in older people, particularly those with long-term health and mobility problems.
Bowel incontinence is less common than urinary incontinence.
It can be very embarrassing and can cause difficulties in leading normal daily life.
Bowel incontinence usually needs to be investigated by a specialist to find out what's causing it. There are treatments available to ease symptoms and sometimes cure the problem altogether.
Causes
You control when you go to the toilet using muscles (called sphincter muscles) and nerves in and around the rectum and anal canal. When you need to pass a stool, the nerves send a message to the sphincter muscles telling them to relax and open the anus.
If this is inconvenient, for example, because you cannot get to a toilet, the brain sends a message to stop the muscles relaxing. You usually aren't aware of doing this until the rectum becomes very full and a conscious effort is needed to keep the anus closed.
If the muscles and nerves do not work properly, bowel incontinence can develop. This can be caused by a number of factors:
- Diet: Anything that makes your faeces more liquid - for example, beer - can make it harder to hold in. Foods that increase flatulence (wind) can also cause leakage, as the anus has to relax to let out gas.
- Irritable bowel syndrome (IBS): In IBS the bowel muscle is very sensitive and squeezes very strongly, which can be hard to control. You may find you have to rush to the toilet when you have the urge to pass stools, or even when you pass wind, as this can sometimes cause leakage.
- Childbirth: After childbirth, one in ten women has problems controlling when they pass wind or stools. It's more common in older mothers (35 and over), and women who have large babies. The problem can develop if the anal muscle tears during birth, or because of the episiotomy cut that is made to help deliver the baby.
- Age: The sphincter muscles get weaker with age, which can make it harder to control when you go to the toilet. Older people with mental health conditions such as dementia may also have trouble recognizing when they need to pass stools.
- Constipation: Constipation happens when hard faeces build up in the lower bowel. Watery faeces can leak round them and be difficult to control. Constipation is often the real cause of bowel incontinence especially in elderly people.
- Medication: Certain medications, for example those containing magnesium trisilicate, make the faeces looser or cause diarrhoea. Over-use of laxatives can also have this effect. Consult your GP if you think your medication could be causing the problem, as they may be able to suggest an alternative.
- Diarrhea: Loose stools are more difficult to control than solid stools.
- Injury or damage to the sphincter muscles or nerves: This can happen during childbirth, following surgery, or because of neurological (nervous system) conditions such as stroke, epilepsy and multiple sclerosis.
- Lower bowel disorders: Conditions such as hemorrhoids, cancer and anal fistula/ fissure can also lead to bowel incontinence.
Diagnosis
The clinical diagnosis is by history and examination where a rectal examination is done by the doctor with a finger to check for the strength of the muscle. It can give the doctor a lot of information. Using some lubricant, the doctor will gently insert a gloved finger into your anus to feel for lumps or bumps. The procedure is not painful, but it can make you feel as if you want to go to the toilet.
Your doctor may also suggest using a hollow, lighted tube called a proctoscope to look at the bowel lining and rectal wall more closely.
If these tests cannot be done in the clinic you may be referred to your local hospital.
Another test that may be needed is a sigmoidoscopy. A thin, rigid tube called a sigmoidoscope is gently inserted through your rectum into the lower part of the bowel. The sigmoidoscope is fitted with a light and a camera which allows the doctor to look for inflammation, tumors, or other problems.
Anorectal physiological studies or anal ultrasound are two further tests that may be done. Anorectal physiological studies test how the nerves and muscles around the anus and rectum are working. Anal ultrasound is a type of scan that uses sound waves to form an image of the muscles around the anal canal. Both tests are outpatient appointments.
Treatment
There are several treatments for bowel incontinence depending on the cause of the problem. Non-surgical treatments include:
- Medication: Drugs can help mild bowel incontinence that happens from time to time. Bowel incontinence that is caused by loose stools, weak sphincter muscles, or over-squeezing bowel muscles can be treated in this way. Medication may help to reduce contractions (squeezing) of the large bowel, and/or increase absorption of fluids so that stools are more solid
- Pelvic floor exercises: Pelvic floor exercises can help to strengthen the muscles around the rectum and anus so that you can control bowel movements more easily.
- Diet: If bowel incontinence is caused by constipation, changing your diet to include more fiber can help. Fiber-rich foods soften the stools by absorbing water and help waste products to pass through the digestive system more easily. Good sources include whole meal bread, brown rice, fruit, and vegetables.
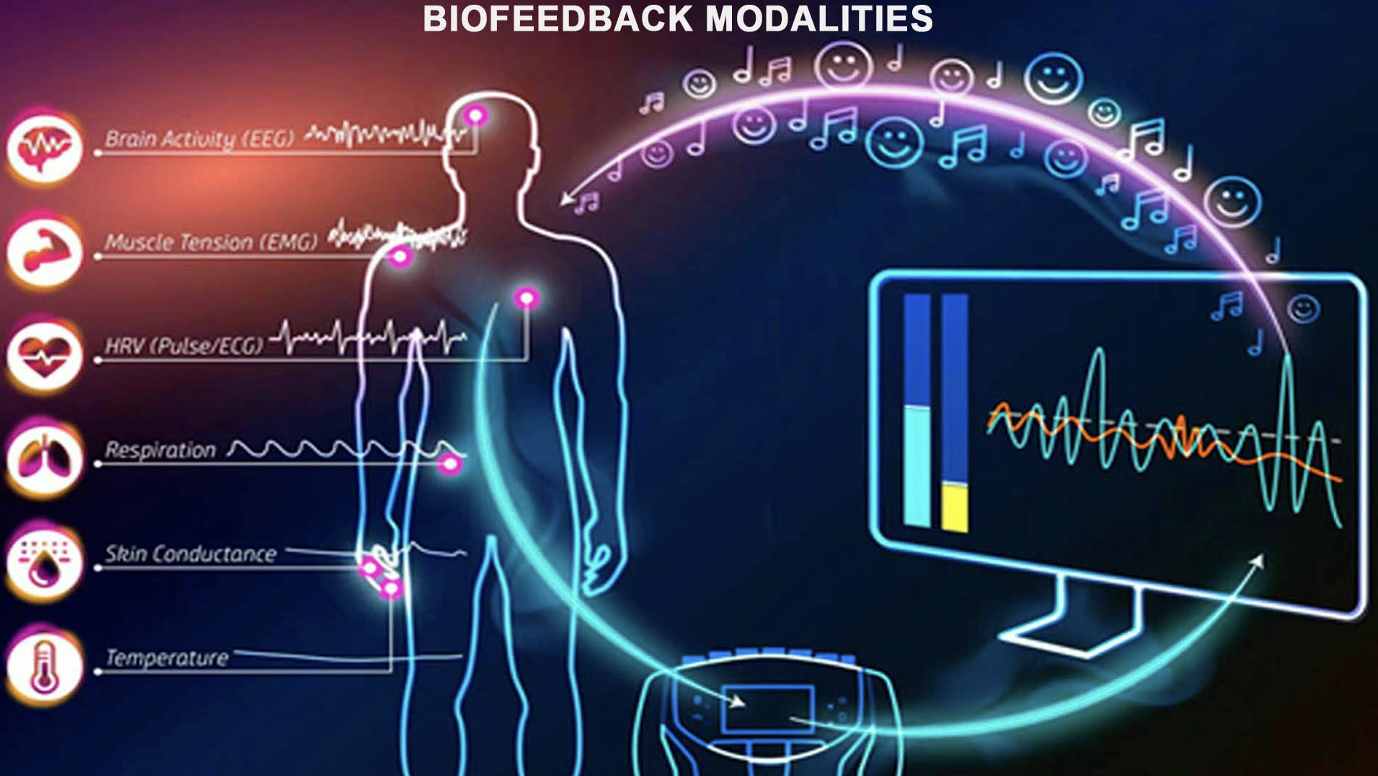
- Biofeedback: This is a behavioral treatment that helps you to identify the feeling of a full rectum and to resist the immediate desire to rush to the toilet. This trains the sphincter muscles to contract when necessary.ccc
If the above treatments do not help to mange bowel incontinence, you may need surgery.
Non-Surgical Irrigation Systems

Surgical Option
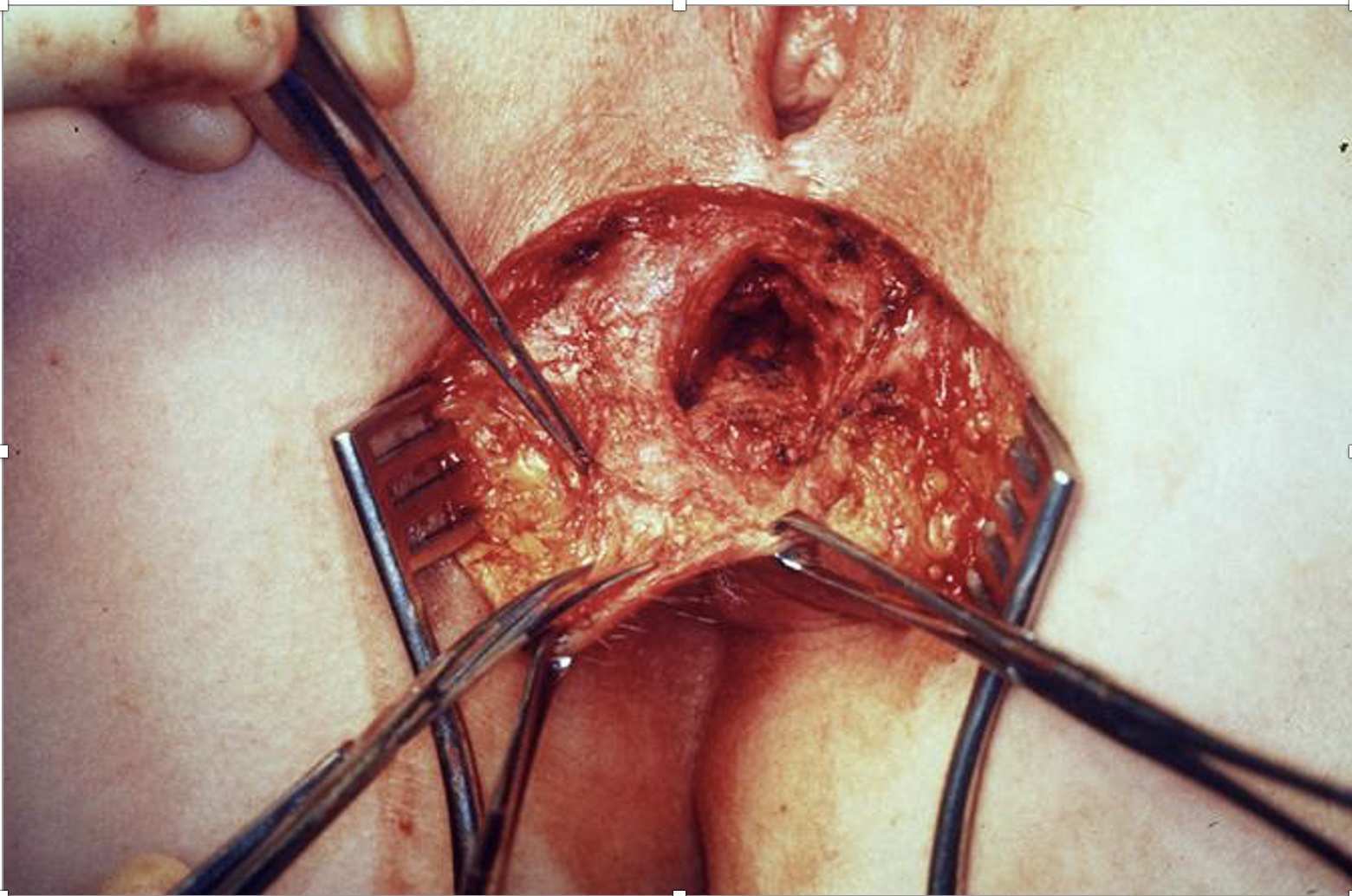
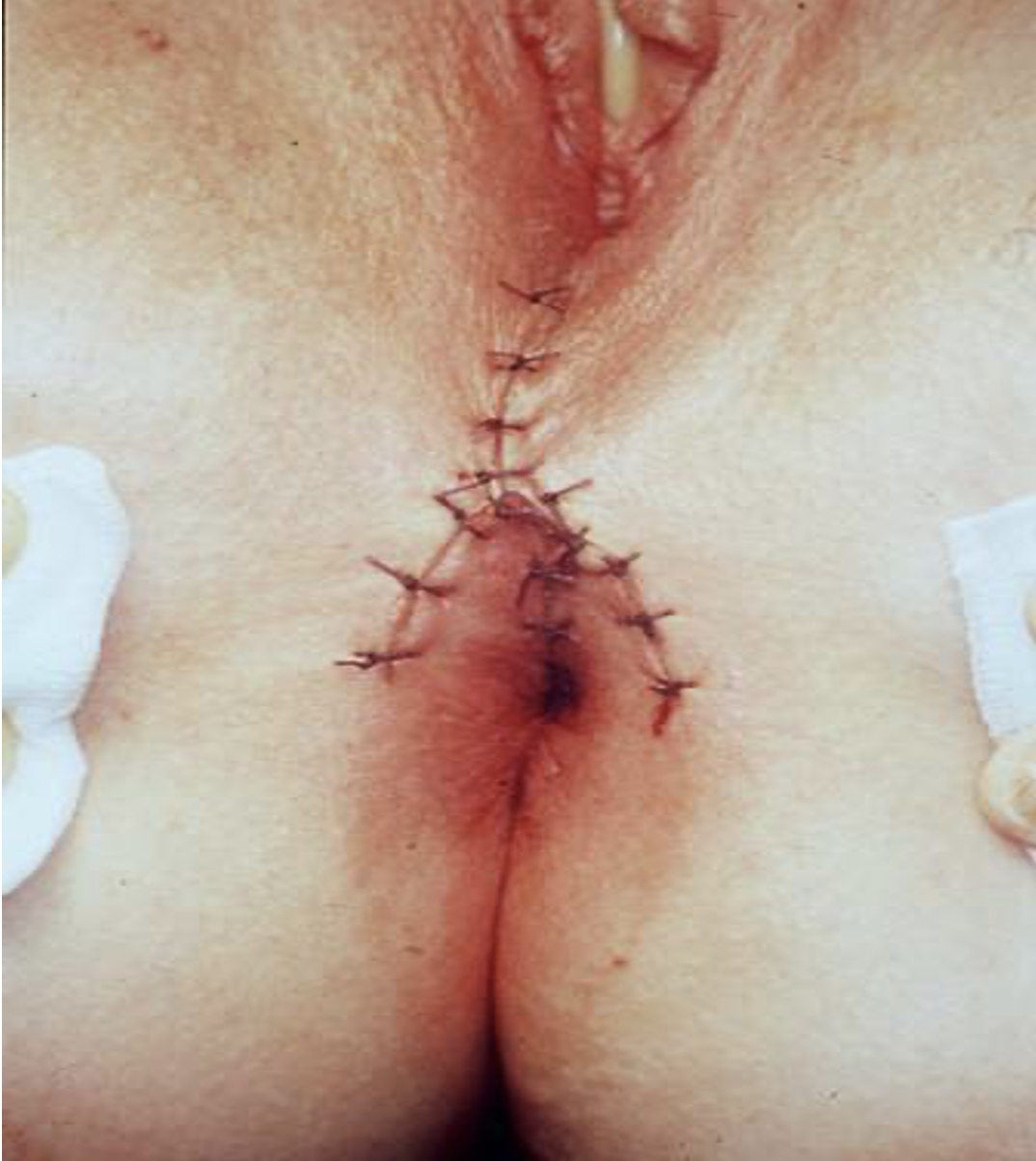
Sphincter repair
Sphincter repair is the most performed surgery. This is mainly done for isolated sphincter injuries post-delivery or traumatic.
The results are better the earlier they are done after damage
This can be combined with levatorplasty for better results
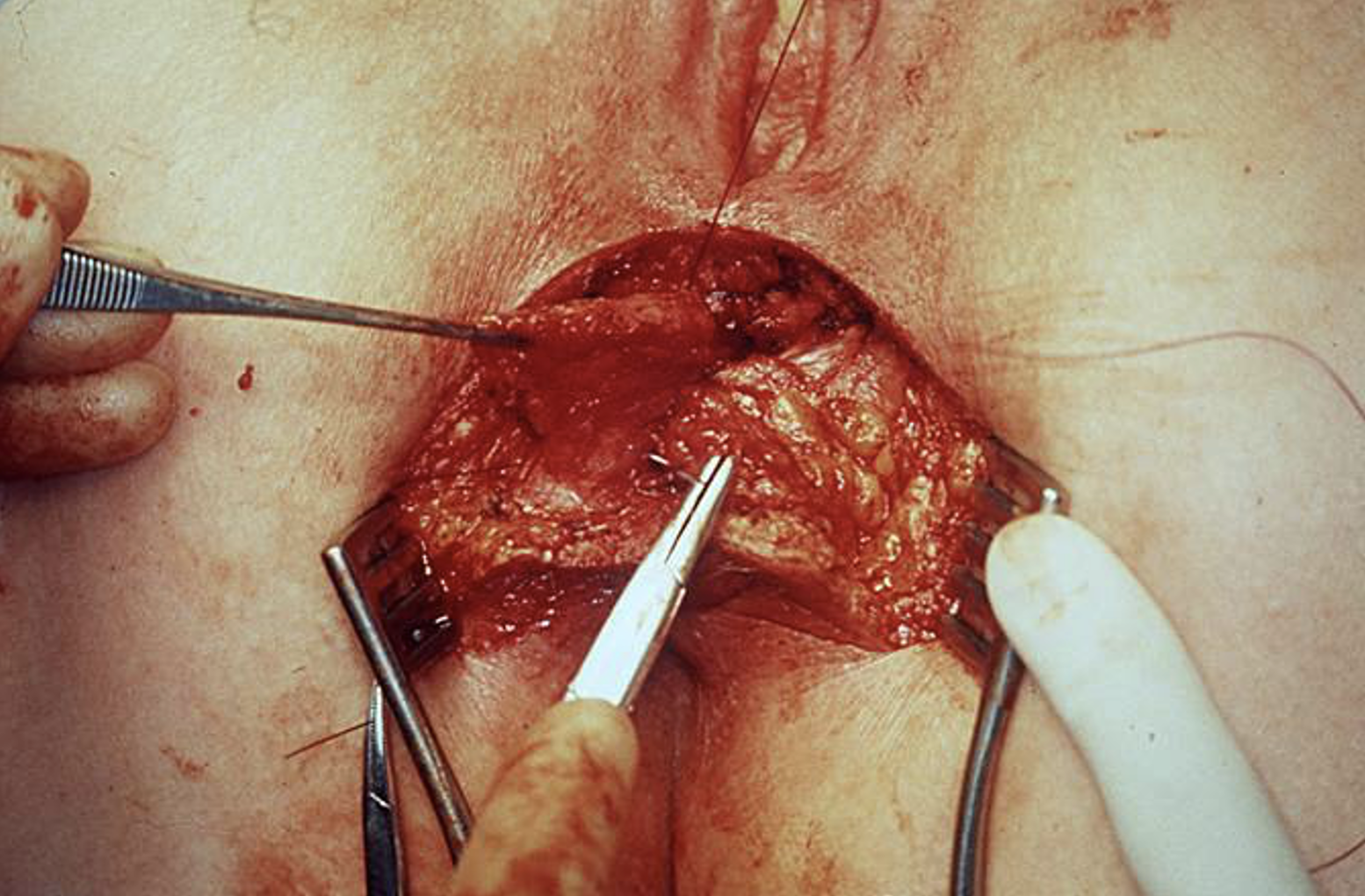
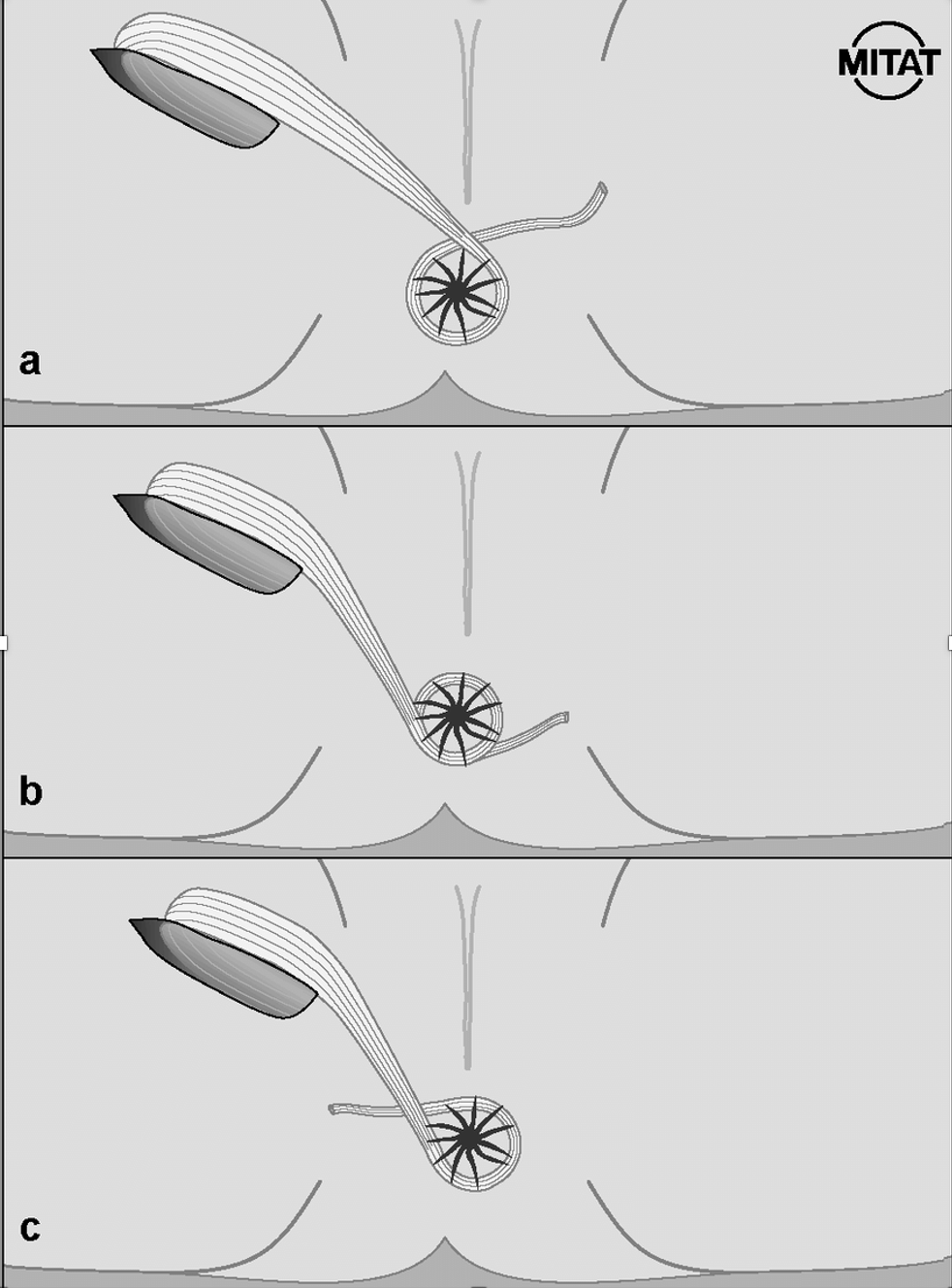
Gracilis Muscle Interposition and Wrap
This is done for patients with muscle mass loss or significant damage of muscle greater than 120 degree
Here a muscle from the leg is removed and moved to surround the anal canal.
This can improve your function. this is also used when there is absence of perineal body
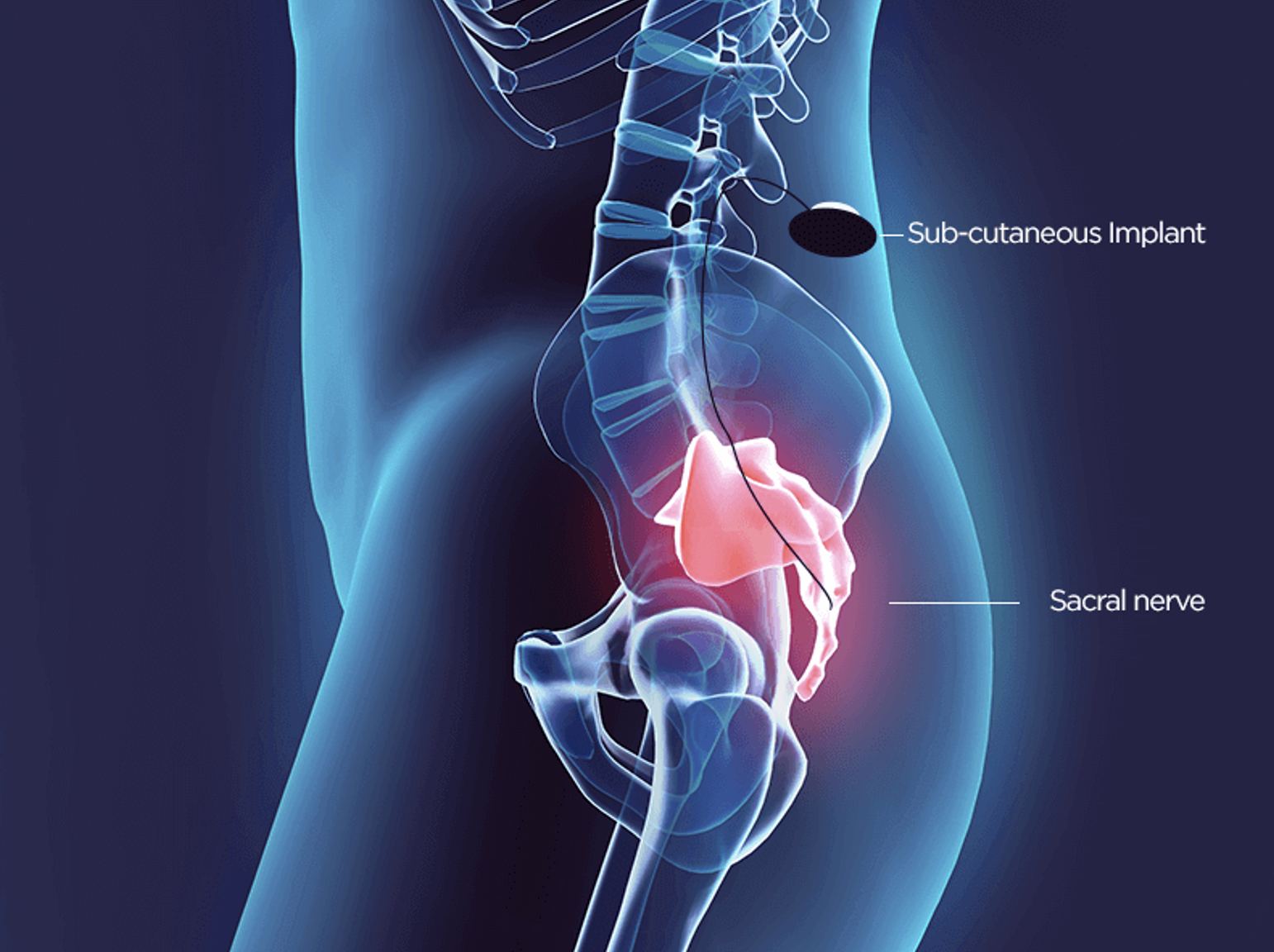
Sacral Nerve Stimulation
For patients who have a poor sphincter or with multiple injuries and those who have a poor response to surgery can have an implant placed like a cardiac pacemaker which constantly keeps your continent by stimulating the nerve and keeping the back passage closed
This procedure has very good success rates and is a backup procedure with very good results
Success in rates of 85-95% have been reported